Blue Nevus excision from thumb nail
-

Blue Nevus Thumb Nail - Nailplate being removed
-
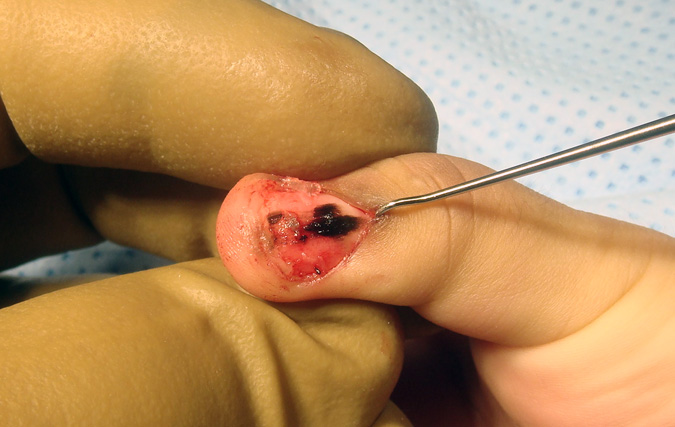
Blue Nevus Thumb Nail - melanotic changes in sterile matrix
-

Blue Nevus Thumb Nail - Partial excision of melanotic area
-

Blue Nevus Thumb Nail-Sterile matrix repair and germinal matrix preserved
