Brachial Plexus Related Diagrams
-
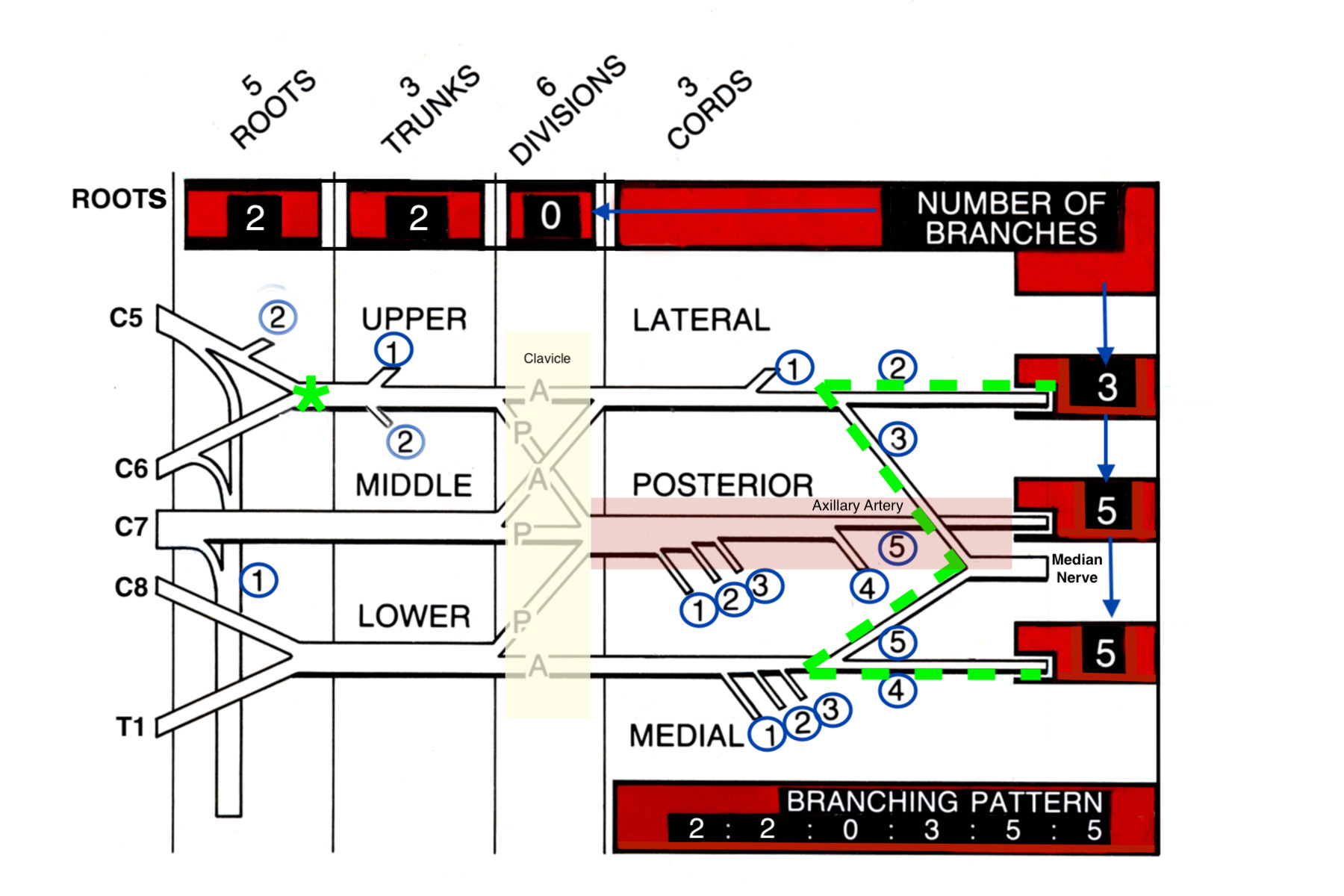
Brachial Plexus diagram showing roots, trunks, divisions & cords. (Remember RTDCBs - Running Together Down Country Byways). Also note the Nerve Branching 2 2 0 3 5 5 Rule for the number of branches from each part of the plexus. Also see the brachial plexus branching table in the next image. Note the green asterisk at Erb’s point. Also note the brachial plexus “M” landmark shape anterior to the axillary artery which is defined by the musculocutaneous nerve, the median nerve and the ulnar nerve. Finally note the divisions of the brachial plexus posterior to the clavicle.
-
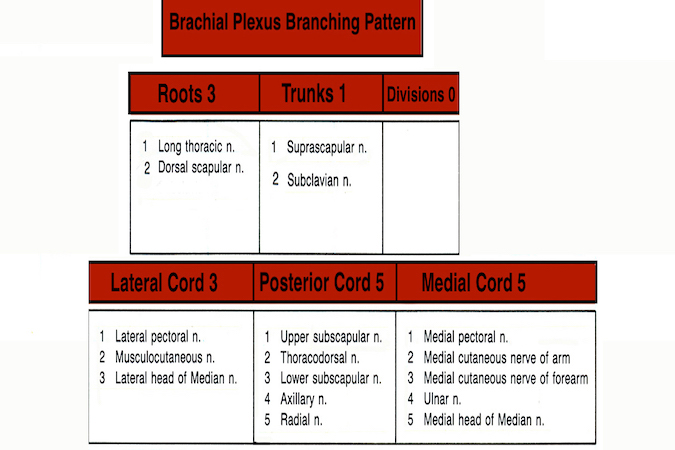
Brachial Plexus Branching Pattern
-
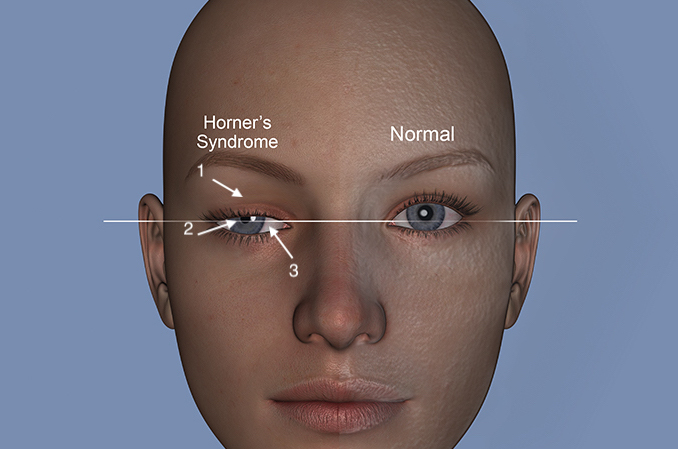
Horner’s sign is frequently associated with C8 and T1 root avulsions which also damage the sympathetic fibers to the face and may produce an ipsilateral Horner’s sign: 1) Ptosis (drooped eyelid); 2) meiosis (constricted pupil); 3) enophthalmos (sunken globe). Horner’s sign is associated with anhydrous of the ipsilateral face and a poor prognosis when connected with a brachial plexus injury.
