Complex Regional Pain Syndrome Clinical Presentation
-
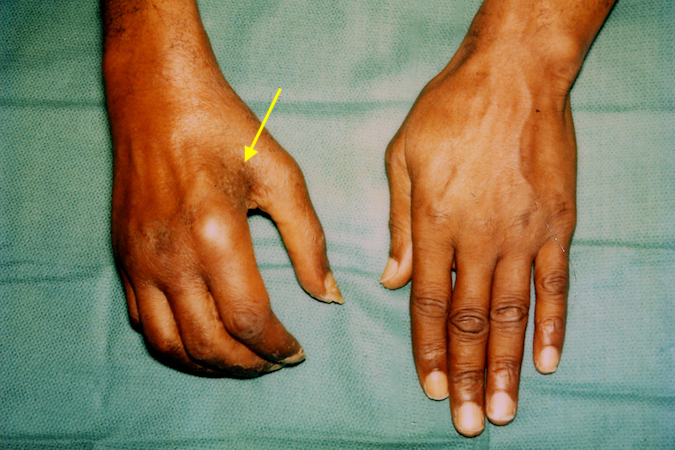
Complex Regional Pain Syndrome Type II in a 46 y.o. male after a bicycle accident and a closed injury to the ulnar nerve at the elbow. Note the intrinsic atrophy (arrow), swollen and stiff hand.
-
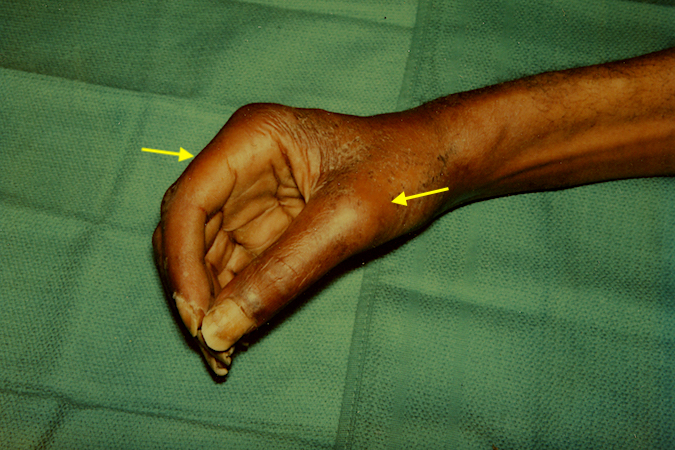
Note the marked lack of active finger flexion and redness (arrows).
