Fracture Nomenclature for Pediatric Distal Radius Salter I-V Fractures
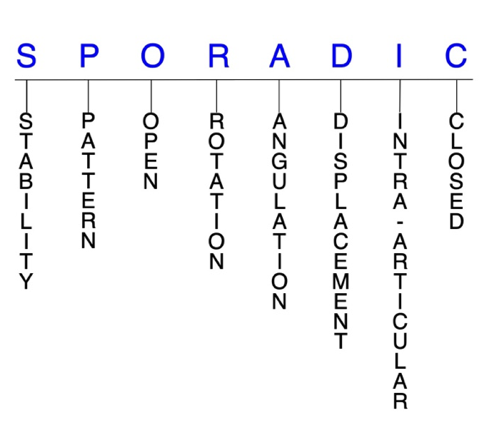
Hand Surgery Resource’s Diagnostic Guides describe fractures by the anatomical name of the fractured bone and then characterize the fracture by the Acronym:
In addition, anatomically named fractures are often also identified by specific eponyms or other special features.
For the Pediatric Distal Radius Salter I-V Fracture, the historical and specifically named fractures include:
None
By selecting the name (diagnosis), you will be linked to the introduction section of this Diagnostic Guide dedicated to the selected fracture eponym.
Although the bones of adults and children share many of the same risks for fracture, children are uniquely susceptible to physeal fracture, as their bones are still growing, and the growth plate is the weakest part of the growing bone. Growth plates are located at the ends of the long bones, and they help determine the ultimate length and shape of mature bones. Thus, these fractures require prompt attention. If not treated properly, an arm or leg could grow to be crooked or of unequal length compared to the other limb. In 1963, Salter and Harris proposed a classification system for pediatric physeal fractures. The Type II fracture is the most common type of physeal fracture. In the Salter/Harris classification, the higher the number, the more likely the growth plate will be permanently damaged and bone deformity will occur.
Definitions
- A pediatric distal radius fracture is a disruption of the mechanical integrity of the distal radius.
- A pediatric distal radius fracture produces a discontinuity in the distal radius contours that can be complete or incomplete.
- A pediatric distal radius fracture is caused by a direct force that exceeds the breaking point of the bone.
Hand Surgery Resource’s Fracture Description and Characterization Acronym
SPORADIC
S – Stability; P – Pattern; O – Open; R – Rotation; A – Angulation; D – Displacement; I – Intra-articular; C – Closed
S - Stability (stable or unstable)
- Universally accepted definitions of clinical fracture stability is not well defined in the literature.1-3
- Stable: fracture fragment pattern is generally nondisplaced or minimally displaced. It does not require reduction, and the fracture fragments’ alignment is maintained by with simple splinting or casting. However, most definitions define a stable fracture as one that will maintain anatomical alignment after a simple closed reduction and splinting. Some authors add that stable fractures remain aligned, even when adjacent joints are put to a partial range of motion (ROM).
- Unstable: will not remain anatomically or nearly anatomically aligned after a successful closed reduction and immobilization. Typically, unstable pediatric distal radius fractures have significant deformity with comminution, displacement, angulation, and/or shortening.
- A pediatric distal radius fracture is further defined as unstable if it is unable to resist displacement after being anatomically reduced.4
P - Pattern
- Distal radial styloid
- Distal dorsal medial fragment
- Distal volar medial fragment
- Distal radial shaft
O - Open
- Open: a wound connects the external environment to the fracture site. The wound provides a pathway for bacteria to reach and infect the fracture site. As a result, there is always a risk for chronic osteomyelitis. Therefore, open fractures of the pediatric distal radius require antibiotics with surgical irrigation and wound debridement.1,5,6
R - Rotation
- Pediatric distal radius fracture deformity can be caused by proximal rotation of the fracture fragment in relation to the distal fracture fragment.
- Degree of malrotation of the fracture fragments can be used to describe the fracture deformity.
A - Angulation (fracture fragments in relationship to one another)
- Angulation is measured in degrees after identifying the direction of the apex of the angulation.
- Straight: no angulatory deformity
- Angulated: bent at the fracture site
- Extreme dorsal angulation may be associated with triangular fibrocartilage complex (TFCC) injuries.4
D - Displacement (Contour)
- Displaced: disrupted cortical contours
- Nondisplaced: ≥1 fracture lines defining one or several fracture fragments; however, the external cortical contours are not significantly disrupted
- In pediatric distal radius fractures, displacement can be either extra-articular or intra-articular. Extra-articular displacement can occur in any of the 3 planes. When displacement occurs in the sagittal plane, it typically leads to loss of the palmar tilt, while volar shear injuries tend to increase palmar tilt. In the coronal plane, displacement typically manifests as the loss of radial inclination and/or height.7
I - Intra-articular involvement
- Intra-articular fractures are those that enter a joint with ≥1 of their fracture lines.
- Distal radius fractures can have fragment involvement with the radiocarpal joint or distal radioulnar joint (DRUJ).
- If a fracture line enters a joint but does not displace the articular surface of the joint, then it is unlikely that this fracture will predispose to post-traumatic osteoarthritis. If the articular surface is separated or there is a step-off in the articular surface, then the congruity of the joint will be compromised and the risk of post-traumatic osteoarthritis increases significantly.
C - Closed
- Closed: no associated wounds; the external environment has no connection to the fracture site or any of the fracture fragments.4-6
Related Anatomy8,9
- The radius consists of a radial head and radial neck at its proximal end. The shaft of the radius then extends from the neck and has a rectangular epiphysis on its distal end. The articular—or lateral—surface of the distal radius is biconcave and triangular, and the apex of this triangle is directed toward the styloid process. On the medial surface, there is a concavity called the ulnar notch that articulates with the head of ulna, forming the DRUJ. The distal surface of the radius has two facets for articulation with the scaphoid and lunate carpal bones. There is also an articulation between the distal radius and the triquetral bone facilitated by a biconcave articular disc. Collectively, these three articulations form the radiocarpal joint.
- Ligaments associated with the distal radius include the dorsal radiocarpal ligament, which spans the ulnar aspect of the dorsal rim of the distal radius from the ulnar margin of the Lister tubercle to the sigmoid notch; the radioscaphocapitate ligament, which originates from the radial styloid and spans to the volar rim of the distal radius at the scaphoid fossa; the long radiolunate ligament, which originates from the volar rim of the scaphoid fossa; and the short radiolunate ligament, which originates from the volar rim of the lunate fossa.
- Tendons associated with the distal radius include those associated with the extensor carpi radialis brevis (ECRB), extensor carpi radialis longus (ECRL), and EPL muscles. The dorsal tubercle protrudes on the posterior aspect of the distal head of the radius and is seated between the grooves for the tendons of the ECRB and ECRL as well as the tendon of the EPL.
- The radius and ulna are connected by a sheet of thick fibrous tissue called the interosseous membrane.
Incidence
- Salter-Harris type II fractures occur after age 10 years.
- Physeal fractures are twice as likely in boys as in girls, since girls finish growing earlier than boys (14 vs 16 years).
- Approximately 33% of all growth plate fractures occur during competitive sports (e.g., football, basketball, gymnastics), while about 20% occur during recreational sporting activities (e.g., biking, skiing, skateboarding).
