Fracture Nomenclature for Fracture Radius and/or Ulna and/or Both Forearm Bones
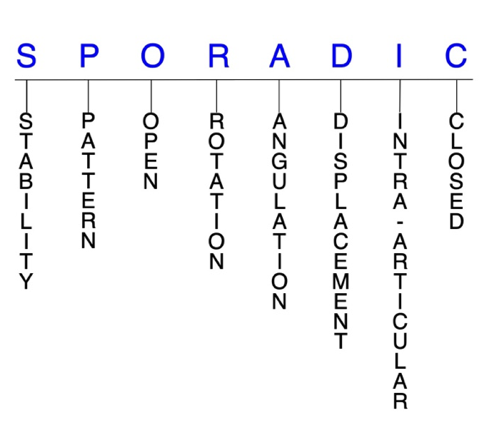
Hand Surgery Resource’s Diagnostic Guides describe fractures by the anatomical name of the fractured bone and then characterize the fracture by the Acronym:
In addition, anatomically named fractures are often also identified by specific eponyms or other special features.
For the Fracture Radius and/or Ulna and/or Both Forearm Bones, the historical and specifically named fractures include:
Galeazzi fracture
Monteggia fracture
By selecting the name (diagnosis), you will be linked to the introduction section of this Diagnostic Guide dedicated to the selected fracture eponym.
Radial and ulnar shaft fractures are relatively common injuries. Although either the radial shaft or ulnar shaft can be fractured in isolation, in most cases both bones are injured simultaneously, and these are referred to as “both bone forearm fractures.” There is a bimodal age distribution for forearm fractures, with one peak in teenage male patients and another in women over the age of 60 years. In adults, these injuries are typically due to motor vehicle accidents, athletic injuries, and falls from height, while low-energy trauma can also produce a fracture in individuals with impaired bone quality. Although conservative treatment may be indicated in certain cases, the majority of forearm fractures are managed surgically through open reduction and internal fixation (ORIF).1-4
Definitions
- Forearm fractures are a disruption of the mechanical integrity of the radial and/or ulnar shaft.
- Forearm fractures produce a discontinuity in the radial and/or ulnar shaft contours that can be complete or incomplete.
- Forearm fractures are caused by a direct force that exceeds the breaking point of the bone.
Hand Surgery Resource’s Fracture Description and Characterization Acronym
SPORADIC
S – Stability; P – Pattern; O – Open; R – Rotation; A – Angulation; D – Displacement; I – Intra-articular; C – Closed
S - Stability (stable or unstable)
- Universally accepted definitions of clinical fracture stability are not well defined in the literature.5-7
- Stable: fracture fragment pattern is generally nondisplaced or minimally displaced. It does not require reduction, and the fracture fragments’ alignment is maintained with simple splinting or casting. However, most definitions define a stable fracture as one that will maintain anatomical alignment after a simple closed reduction and splinting. Some authors add that stable fractures remain aligned, even when adjacent joints are put to a partial range of motion (ROM).
- Unstable: will not remain anatomically or nearly anatomically aligned after a successful closed reduction and immobilization. Typically unstable radial and ulnar shaft fractures have significant deformity with comminution, displacement, angulation, and/or shortening.
- For radial shaft fractures, the likelihood of instability is higher when the injury site is more distal than proximal.8
- An unstable ulnar shaft fracture is one that involves >50% displacement, >10° angulation, the proximal third of the bone, or which also features proximal radioulnar joint (PRUJ) or distal radioulnar joint (DRUJ) instability. Most ulnar shaft fractures, however, are stable.2
P - Pattern
- Radial shaft
- Proximal third
- Middle third
- Distal third
- Apex volar
- Apex dorsal
- Ulnar shaft
- Proximal third
- Middle third
- Distal third
- Apex volar
- Apex dorsal
O - Open
- Open: a wound connects the external environment to the fracture site. The wound provides a pathway for bacteria to reach and infect the fracture site. As a result, there is always a risk for chronic osteomyelitis. Therefore, open forearm fractures require antibiotics with surgical irrigation and wound debridement.5,9,10
- There is high risk for visible deformity and open injury in both bone forearm fractures due to the significant forces involved.4
- Many isolated ulnar shaft fractures are also open, while open radial shaft fractures are not uncommon.1,2
R - Rotation
- Forearm fracture deformity can be caused by proximal rotation of the fracture fragment in relation to the distal fracture fragment. Rotational deformities are common after forearm fractures.
- Degree of malrotation of the fracture fragments can be used to describe the fracture deformity.
A - Angulation (fracture fragments in relationship to one another)
- Angulation is measured in degrees after identifying the direction of the apex of the angulation.
- Straight: no angulatory deformity
- Angulated: bent at the fracture site
- Galeazzi fractures have been found to result in shortening and angulation, which is responsible for the disruption of the DRUJ.8
D - Displacement (contour)
- Displaced: disrupted cortical contours
- Nondisplaced: ≥1 fracture lines defining one or several fracture fragments; however, the external cortical contours are not significantly disrupted
I - Intra-articular involvement
- Intra-articular fractures are those that enter a joint with ≥1 of their fracture lines.
- Forearm fractures can have fragment involvement with the DRUJ, PRUJ, radiocarpal, humeroulnar, or humeroradial joints.
- If a fracture line enters a joint but does not displace the articular surface of the joint, then it is unlikely that this fracture will predispose to post-traumatic osteoarthritis. If the articular surface is separated or there is a step-off in the articular surface, then the congruity of the joint will be compromised and the risk of post-traumatic osteoarthritis increases significantly.
C - Closed
- Closed: no associated wounds; the external environment has no connection to the fracture site or any of the fracture fragments.4-6
Forearm fractures: named fractures, fractures with eponyms and other special fractures
Galeazzi fracture
- Also known as a reverse Monteggia fracture or Piedmont fracture, the Galeazzi fracture is fracture of the middle to distal third of the radial shaft combined with a subluxation or dislocation of the DRUJ.8,11
- The Galeazzi fracture is considered a true forearm axis injury because concomitant bone and soft tissue injuries—particularly the triangular fibrocartilage complex (TFCC) and/or interosseous membrane (IOM) which contribute to forearm instability.1,8
- These injuries typically result from direct impact to the radius with forearm pronation. When a patient sustains a radial shaft fracture in the middle to distal third of the bone, suspicion should be raised for an associated DRUJ injury.1,8
- Galeazzi and Monteggia fractures—discussed next—are more common in pediatric than adult patients.4
Imaging11
- Radiology studies - X-ray
- Anteroposterior (AP) and lateral views are usually sufficient, but an oblique view may help to better classify the injury.
- If a coexistent injury is suspected, the distal wrist and proximal elbow should also be radiographed.
- Radiology studies - Computerized tomography (CT) scanning
- Not usually needed, but occasionally used to evaluate for nonunion.
- Magnetic resonance imaging - MRI without contrast
- Often used to detect TFCC tears and/or IOM disruption.
Treatment
Conservative
- Conservative treatment is not recommended for most adults with Galeazzi fractures; however, temporary immobilization with a sugar-tong splint may be used while a patient is awaiting an orthopedic consult or surgery.11
Operative
- Surgery is required in the majority of cases and first involves rigid fixation of the radius. This is followed by intraoperative assessment of DRUJ stability.
- If the DRUJ is stable after fixation. This may be followed by immobilization in supination or a neutral position for 2-4 weeks.
- If the DRUJ is unstable, the TFCC may be repaired and/or the forearm pinned in supination in a reduced position.8
- If an ulnar styloid fracture accompanies the unstable DRUJ, the styloid should be repaired with fixation using a lag screw, tension band wire or with excision of the fragment and repair of the TFCC to the fovea.8,11
- Volar plate fixation
- Most common surgical approach
- Fixation may be more difficult when the fracture is in the distal third of the radius, where it may only be possible to insert two screws distal to the fracture line in these cases if using a 3.5-mm straight plate.1 Modern T-plates provide better fixation in the distal fragment by allowing additional screws in the distal fragment.
- Open reduction of the DRUJ11
- Sometimes necessary when the DRUJ cannot be reduced closed.
- The TFCC should be repaired and/or the forearm pinned in supination.
- Followed by immobilization with a splint or cast and the elbow in supination.
Complications
- Nonunion
- Malunion
- DRUJ instability
- Reduced grip strength
Outcomes
- Due to their complexity, Galeazzi fractures can lead to a variety of outcomes, and complication rates as high as 40% have been reported.11
- Closed reduction and immobilization alone has been associated with poor outcomes in >90% of adult patients.11
Monteggia fracture
- A Monteggia fracture involves a fracture of the proximal third of the ulna combined with a subluxation or dislocation of the radial head at the PRUJ and the humeroradial joint.4,8
- These injuries most commonly occur secondary to a direct blow to the posterior aspect of the ulna, with the elbow extended and the forearm in hyperpronation.12,13
- Monteggia fractures account for <2% of all forearm fractures.12
Imaging13
