Human Bite Diagrams -Fighter's Bite
-
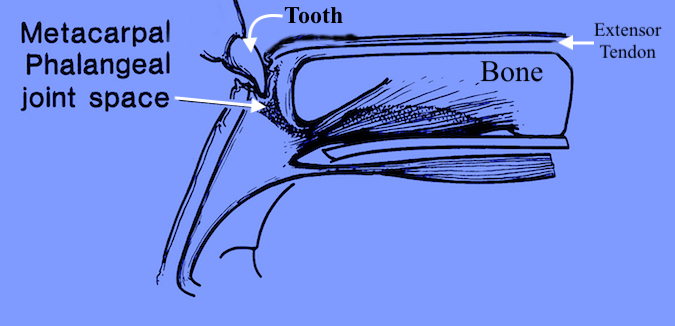
Human Bite - Punch or Fighter's Bite with tooth going through skin, extensor tendon and joint capsule. This inoculates of joint space with bacteria.
-
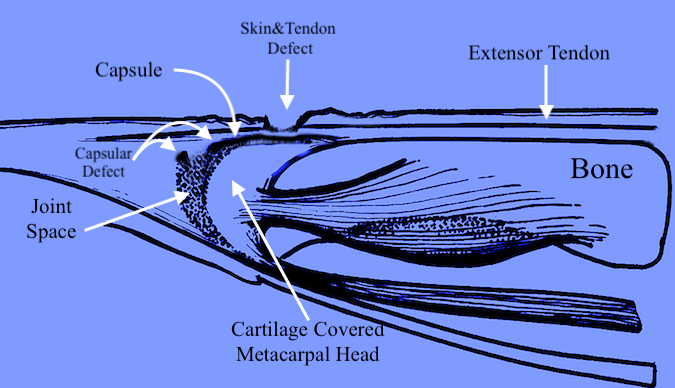
When the patient presents in the ER for examination of the now extended finger, the defect in the skin and extensor tendon has retracted proximally over intact joint capsule thus sealing bacteria in the joint and hiding the capsular defect.
