Spaces, Bursa and Flexor Tendon Sheaths
-

Thumb flexor tendon sheath shown separate but is connect to the radial bursa at the MP joint level and extends proximal to the transverse carpal ligament..
-

Index finger flexor tendon sheath which can connect to the thenar space.
-

Long finger flexor tendon sheath which can connect to the mid-palmar space.
-

Ring finger flexor tendon sheath which can connect to the mid-palmar space.
-
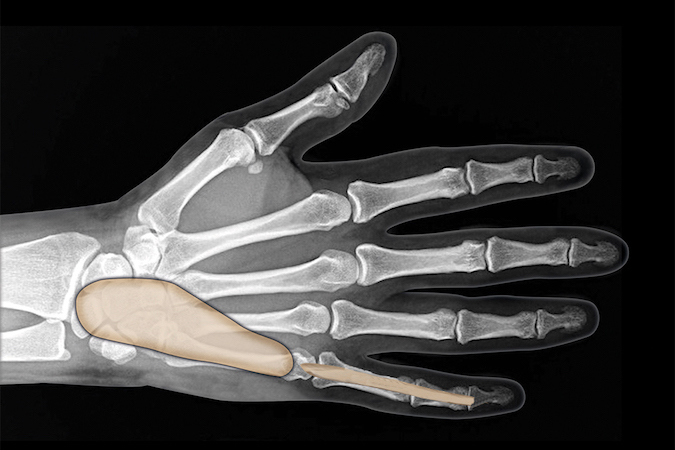
Little finger flexor tendon sheath is usually connect to the ulnar bursa.
-
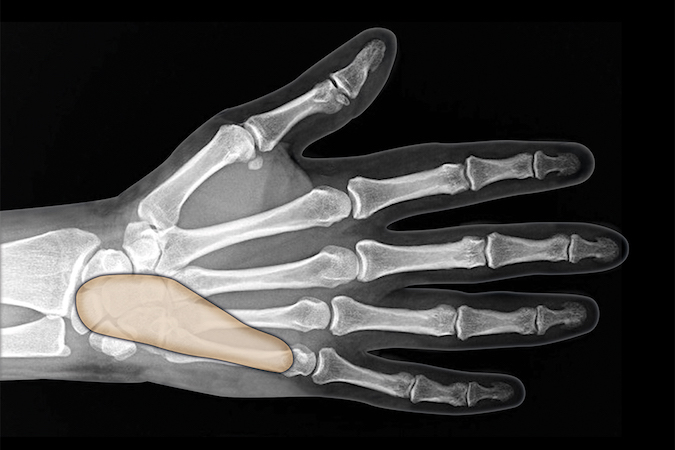
The ulnar bursa which can connect to the radial bursa and flexor sheaths of thumb and little finger to form "horseshoe" abscess.
-
The hypothenar space is a potential space between the combined palmar and superficial hypothenar muscle fascia and the deep hypothenar muscle fascia. Infection is usually secondary to a puncture wound.
-
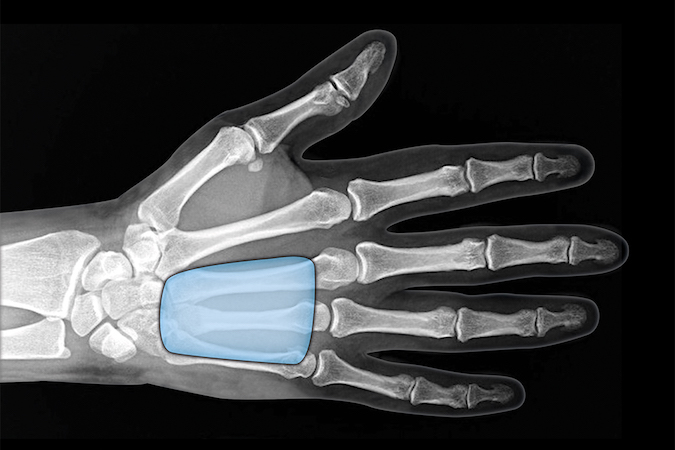
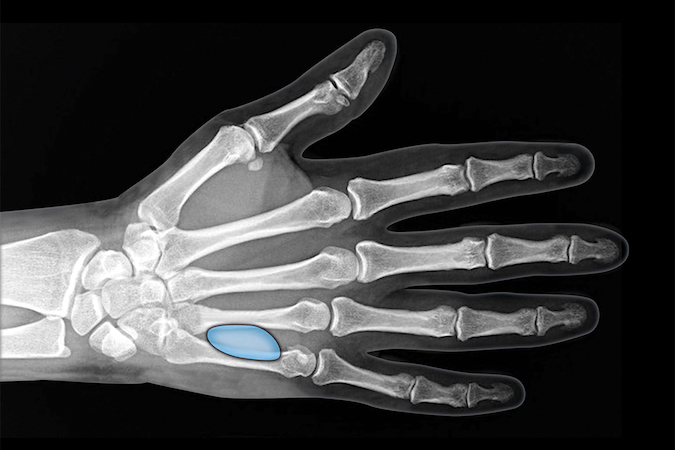
The midpalmar space is a potential space between the volar interosseous fascia, the flexor sheath, the oblique and hypothenar septum. Infection is usually secondary to spread of infection from flexor sheath of long and ring fingers.
-
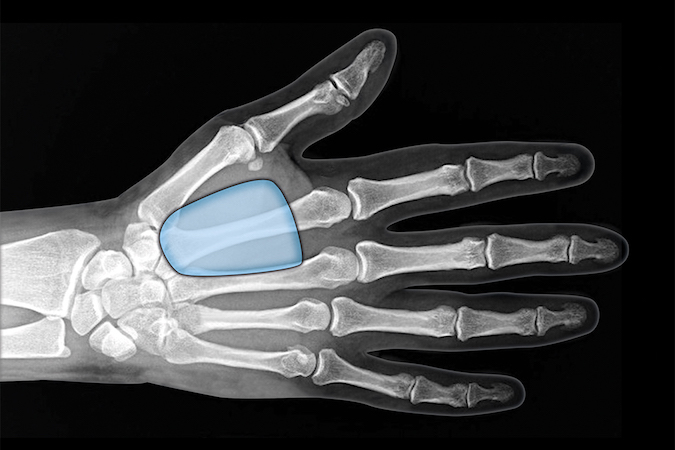
The thenar space is the index flexor sheath and the adductor pollicis fascia. Infection can spread here from the index flexor tendon sheath or from puncture wounds.
-

The Parona Space is superficial to the pronator quadrates and under the flexor tendons. Infection can spread here from the radial or ulnar bursa.
